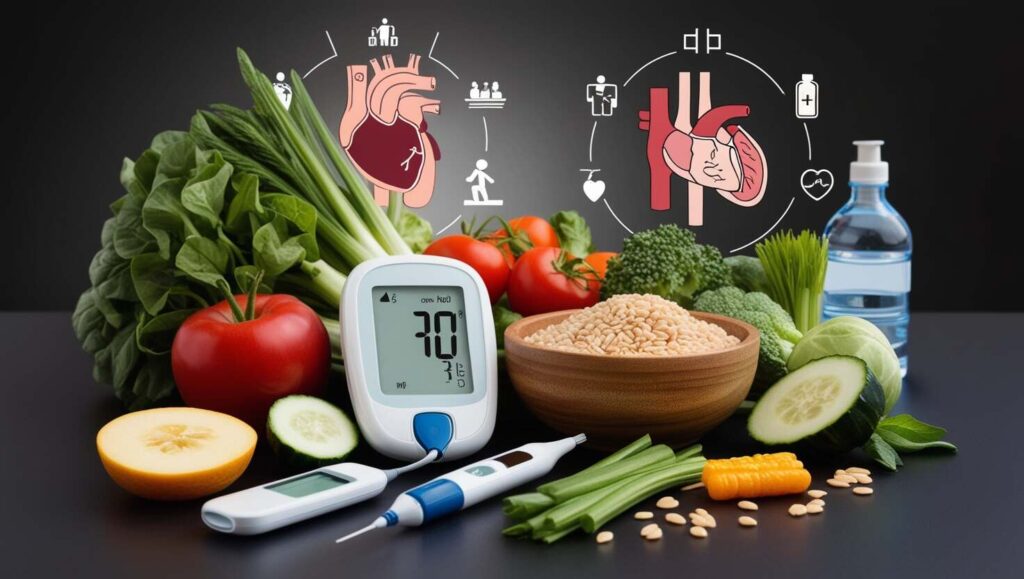
Diabetes is a complex condition affecting millions worldwide, and managing it involves more than just monitoring blood sugar. It touches every aspect of health, from nutrition and lifestyle choices to mental well-being. Understanding diabetes is the first step to effectively managing it, and with the right knowledge, you can make informed decisions that positively impact your life. In this guide, we’ll explore the essential details of diabetes, covering what it is, why it occurs, and how it can be managed for optimal health and wellness because a complete guide is essential to understanding diabetes for optimal health.
What is Diabetes?
Diabetes is a chronic medical condition that occurs when the body either cannot produce enough insulin or cannot effectively use the insulin it produces. Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood sugar (glucose) levels. When insulin is not functioning properly, glucose builds up in the bloodstream, leading to elevated blood sugar levels, which can cause a variety of health problems over time.
The Types of Diabetes
Here are the main types of diabetes:
Type 1 Diabetes
An autoimmune condition where the body’s immune system attacks insulin-producing cells in the pancreas. This leads to very low or no insulin production, requiring daily insulin injections for management. Type 1 diabetes often appears in childhood or adolescence but can occur at any age.
Type 2 Diabetes
The most common form of diabetes, Type 2 occurs when the body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal blood glucose levels. Lifestyle factors, such as diet and exercise, play a significant role in Type 2 diabetes, though genetics can also contribute. This type is typically managed through diet, exercise, medication, and sometimes insulin.
Gestational Diabetes
A form of diabetes that develops during pregnancy in women who have never had diabetes before. Hormones produced during pregnancy can make cells less responsive to insulin, leading to high blood sugar levels. Gestational diabetes usually goes away after pregnancy but increases the risk of Type 2 diabetes later in life.
Prediabetes
A condition where blood sugar levels are higher than normal but not high enough to be diagnosed as diabetes. Prediabetes increases the risk of developing Type 2 diabetes if left unmanaged. However, lifestyle changes such as improved diet, exercise, and weight loss can often reverse prediabetes.
MODY (Maturity Onset Diabetes of the Young)
A rare form of diabetes caused by a genetic mutation, typically diagnosed in young adults and adolescents. Unlike Type 1 and Type 2 diabetes, MODY doesn’t always require insulin and is often managed with lifestyle changes or oral medications.
Secondary Diabetes
A form of diabetes that results from other medical conditions or treatments, such as pancreatic disease, hormonal disorders, or prolonged use of medications like steroids. Managing the underlying condition often helps control blood sugar levels in secondary diabetes.
Each type requires different management approaches, so understanding the specific type of diabetes is crucial for effective treatment and control.
Understanding Blood Sugar Levels
Blood sugar levels fluctuate throughout the day based on what you eat, how much you exercise, and other factors like stress and illness. Here are some key points regarding blood sugar levels:
- Normal Range: A typical fasting blood glucose level is below 100 mg/dL. Levels between 100 and 125 mg/dL indicate prediabetes, while 126 mg/dL or higher suggests diabetes.
- Monitoring: Regular monitoring of blood sugar levels is crucial for managing diabetes. Continuous glucose monitors (CGMs) and fingerstick tests are common methods.
Symptoms of Diabetes
Diabetes symptoms can vary between individuals and may also differ based on the type of diabetes. However, some common symptoms are generally experienced by both men and women. Here’s an overview of the general symptoms of diabetes, along with specific symptoms that may affect men and women.
General Symptoms of Diabetes
Increased Thirst (Polydipsia):
A persistent feeling of thirst that does not go away even after drinking fluids.
Frequent Urination (Polyuria):
Needing to urinate more often than usual, especially at night (nocturia).
Fatigue:
Feeling tired or fatigued, even after getting adequate rest.
Blurred Vision:
Changes in vision due to high blood sugar levels affecting the lenses of the eyes.
Slow-Healing Wounds:
Cuts, sores, or infections that take longer to heal than normal.
Unexplained Weight Loss:
Losing weight without trying, more commonly seen in Type 1 diabetes.
Increased Hunger (Polyphagia):
Experiencing constant hunger despite eating, often due to the body’s inability to use glucose effectively.
Numbness or Tingling:
Feeling numbness or tingling in the hands or feet, which can indicate nerve damage (neuropathy).
Symptoms in Men
Erectile Dysfunction:
Men with diabetes may experience difficulties achieving or maintaining an erection due to nerve and blood vessel damage.
Decreased Libido:
A reduction in sexual desire can occur, often linked to hormonal imbalances or psychological factors related to diabetes.
Skin Infections:
Men with diabetes may be more prone to skin infections, especially fungal infections in warm, moist areas of the body.
Symptoms in Women
Yeast Infections:
Women with diabetes may be more susceptible to yeast infections due to elevated blood sugar levels creating a favorable environment for yeast growth.
Menstrual Irregularities:
Diabetes can lead to changes in menstrual cycles, including heavier periods or missed cycles.
Pregnancy Complications:
Women with diabetes may face complications during pregnancy, including gestational diabetes, high blood pressure, and increased risk of preterm birth.
Complications of Diabetes
Diabetes can lead to a variety of complications that affect different parts of the body. These complications can develop over time, particularly if blood sugar levels are poorly controlled. Here’s an overview of the potential complications associated with diabetes:
Short-Term Complications
Hypoglycemia (Low Blood Sugar):
- Occurs when blood sugar levels drop too low, often due to excessive insulin, missed meals, or intense exercise. Symptoms include shakiness, sweating, confusion, irritability, and in severe cases, loss of consciousness or seizures.
Diabetic Ketoacidosis (DKA):
- Primarily affects individuals with Type 1 diabetes when the body starts breaking down fat for fuel due to a lack of insulin. Symptoms include nausea, vomiting, abdominal pain, rapid breathing, and a fruity-smelling breath. DKA is a medical emergency.
Hyperglycemic Hyperosmolar State (HHS):
- A serious condition mainly associated with Type 2 diabetes, where extremely high blood sugar levels lead to dehydration and confusion. Symptoms include excessive thirst, frequent urination, and dry mouth.
Long-Term Complications
Cardiovascular Disease:
- Diabetes significantly increases the risk of heart disease, stroke, and high blood pressure. The risk is heightened by factors such as high cholesterol, obesity, and inactivity.
Nerve Damage (Neuropathy):
- High blood sugar can damage the nerves, particularly in the legs and feet, leading to symptoms such as pain, tingling, and numbness. This can increase the risk of injuries and infections.
Kidney Damage (Diabetic Nephropathy):
- Diabetes can cause damage to the kidneys’ filtering system, leading to kidney disease or kidney failure. Symptoms may not appear until significant damage has occurred.
Eye Damage (Diabetic Retinopathy):
- High blood sugar can damage the blood vessels in the retina, potentially leading to vision loss or blindness. People with diabetes are also at risk for cataracts and glaucoma.
Foot Damage:
- Nerve damage and poor circulation can lead to foot problems, including infections, ulcers, and, in severe cases, amputations. Proper foot care is essential for individuals with diabetes.
Skin Conditions:
- Diabetes can increase the risk of various skin issues, including bacterial and fungal infections, and diabetic dermopathy (light brown, scaly patches).
Dental Issues:
- Diabetes can lead to gum disease and other dental problems due to reduced blood flow and higher sugar levels in saliva, which can promote bacterial growth.
Mental Health Issues:
- Individuals with diabetes are at a higher risk for depression, anxiety, and eating disorders, which can complicate disease management.
Managing Diabetes
Managing diabetes effectively requires a combination of lifestyle changes and medical interventions. Here are key strategies:
1. Healthy Eating
A balanced diet plays a crucial role in diabetes management. Focus on:
- Whole Foods: Incorporate fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Portion Control: Monitor portion sizes to maintain healthy blood sugar levels.
- Limit Sugar and Refined Carbs: Reduce intake of sugary snacks, desserts, and white bread.
2. Regular Exercise
Physical activity helps regulate blood sugar levels, improves insulin sensitivity, and contributes to weight management. Aim for at least 150 minutes of moderate aerobic activity per week, such as brisk walking, swimming, or cycling.
3. Medication Management
For some individuals, medication or insulin therapy is necessary to control blood sugar levels effectively. Work with your healthcare provider to determine the best approach for your needs.
4. Regular Monitoring
Keep track of your blood sugar levels and maintain regular check-ups with your healthcare team. This will help you adjust your management plan as needed.
Conclusion
A complete guide to understanding diabetes is crucial for effective management and prevention of complications. With the right information, lifestyle changes, and medical support, individuals living with diabetes can lead healthy, fulfilling lives.
FAQs
What is the difference between Type 1 and Type 2 diabetes?
- Type 1 diabetes is an autoimmune condition where the body cannot produce insulin, while Type 2 diabetes is often related to insulin resistance and lifestyle factors.
How can I prevent Type 2 diabetes?
- Preventing Type 2 diabetes involves maintaining a healthy weight, eating a balanced diet, and staying active through regular exercise.
What are the best foods for managing diabetes?
- Foods rich in fiber, lean proteins, healthy fats, and low in refined sugars are ideal for managing blood sugar levels.
How often should I check my blood sugar?
- The frequency of blood sugar monitoring depends on your treatment plan. Consult your healthcare provider for personalized recommendations.
Can diabetes be reversed?
- While Type 2 diabetes may be managed and, in some cases, reversed with lifestyle changes, Type 1 diabetes currently has no cure.
Stay informed, monitor your health, and make proactive choices to manage your diabetes successfully.




6 Comments
An incredibly informative guide! Understanding diabetes and its impact on health is crucial, and this post covers it all. Great resource for anyone looking to manage or learn more about diabetes.
The blog post explore the essential details of diabetes, covering what it is, why it occurs, and how it can be managed for optimal health.
A comprehensive guide to diabetes management—learn essential tips on diet, exercise, and monitoring to improve health and control diabetes effectively.
This guide provides comprehensive and valuable information about understanding diabetes. The tips and insights are well-organized and easy to follow, making it a great resource for managing the condition.
This guide to understanding diabetes and health is incredibly informative! A must-read for anyone looking to gain a clear perspective on managing and preventing diabetes.
Very informative and well-explained! This guide provides a clear understanding of diabetes and how to maintain good health. A must-read for everyone!